- Research
- Open access
- Published:
Lipid-encapsulated gold nanoparticles: an advanced strategy for attenuating the inflammatory response in SARS-CoV-2 infection
Journal of Nanobiotechnology volume 23, Article number: 15 (2025)
Abstract
Background
Nanodrugs play a crucial role in biomedical applications by enhancing drug delivery. To address safety and toxicity concerns associated with nanoparticles, lipid-nanocarrier-based drug delivery systems have emerged as a promising approach for developing next-generation smart nanomedicines. Ginseng has traditionally been used for various therapeutic purposes, including antiviral activity. This study aimed to prepare a biocompatible and therapeutically potent Korean ginseng nanoemulsion (KGS-NE) using ginseng seed oil (GSO), optimize its encapsulation and drug delivery efficiency, and evaluate its antiviral activity.
Results
Various techniques were utilized to confirm the KGS-NE formation. Energy-dispersive X-ray spectroscopy identified gold nanoparticles with the highest Au peak at 2.1 keV. Selected area diffraction patterns revealed crystallographic structures. FT-IR spectrometry detected functional groups, with peaks at 2922.09 cm−1 (alkene C–H stretching), 1740.24 cm−1 (aldehyde C=O stretching), and 1098.07 cm−1 (C–O stretching in secondary alcohol). Storage stability studies showed that KGS-NE maintained its size and stability for 6 months at 4 °C. The KGS-NE exhibited a dose-dependent suppression of HCoV-OC43 viral replication in Vero E6 cells. RNA sequencing analysis unveiled differentially expressed genes (DEGs) specifically involved in the ABC transporters signaling pathway. KGS-NE oral administration facilitated the recovery of mice induced with the receptor binding domain (RBD) of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein, as confirmed by inflammatory markers expression in lung tissue. In the Syrian hamster infected with the SARS-CoV-2 model, the lungs dissected showed enlarged morphology and induced inflammatory cytokines. This effect was mitigated with KGS-NE oral administration, as observed through H&E and qRT-PCR analysis. Biochemical analysis at various oral administration concentrations demonstrated that KGS-NE had no adverse effects on the kidney and liver.
Conclusions
Our findings strongly suggest that oral administering KGS-NE in mice and Syrian hamster models has the potential to effectively mitigate lung inflammation against coronavirus. This indicates a promising new strategy for developing the antiviral nano-agent against SARS-CoV-2.
Graphical Abstract

Introduction
The global health emergency status related to the coronavirus disease 2019 (COVID-19) pandemic has been lifted [1]. However, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus continues to result in fatalities and undergo genetic variations. Oral medications play a crucial role due to their convenience and enhanced patient compliance compared to injectable drugs that may require more medical supervision [2]. Some drugs have received approval from the Food and Drug Administration (FDA) and demonstrated high efficacy in preventing symptoms caused by SARS-CoV-2, such as intravenous drug remdesivir and oral drugs molnupiravir and paxlovid [3]. Concerns about teratogenicity have been raised for molnupiravir, and there is a lack of extensive long-term safety data [4]. Paxlovid faces challenges related to significant drug interactions, potential hepatotoxicity, and accessibility issues due to its cost, necessitating careful consideration for widespread use in managing COVID-19 [5]. Therefore, there is an urgent need to develop low side effects oral drugs for treating COVID-19.
Nanodrug (ND) delivery systems for oral administration can enhance drug bioavailability and targeted delivery [6]. This technology protects sensitive bioactive compounds and aids in overcoming biological barriers, improving therapeutic efficacy [7]. NDs synthesized using metal nanoparticles, such as gold, silver, and platinum, have demonstrated various advantages in biomedical applications, including treatment of COVID-19 [8]. Some reports suggest that metal nanoparticles loaded with bioactive compounds significantly enhance their antiviral activity [9]. However, concerns have been raised about maintaining the stability of these nanoparticles under different conditions. Recent developments include using lipid nanocarriers to facilitate enhanced drug stability and therapeutic efficacy [10]. It provides a stable platform for encapsulating nanoscale drug particles, ensuring improved bioavailability. This approach holds great promise in drug research, offering innovative solutions for targeted drug delivery and addressing challenges associated with traditional drug formulations. Additionally, they are feasible for oral administration due to their high absorption rates, enhancing drug solubility and stability, making them a suitable carrier for oral administration, thereby improving the overall bioavailability of encapsulated NDs.
Lipid nanocarriers exhibit excellent functionality in emulsion-based encapsulation of bioactive compounds [11]. They are less toxic and hold significant potential in industrial applications due to their biocompatibility and stability [12]. The appropriate selection of oil for synthesizing emulsion is pivotal for achieving stability and the desired characteristics [13]. In recent years, edible oils have garnered increasing attention in the formulation of nanoemulsions due to their heightened safety profile and easy accessibility [14]. Edible oils from food sources play a pivotal role in attaining the requisite stability, bioavailability, and other critical attributes in nanoemulsion formulations [15]. Previous studies have demonstrated the application of oils such as sunflower seed oil, olive oil, soybean oil, and rapeseed oil in the preparation of nanoemulsions [16]. Similarly, in recent years, ginseng seed oil (GSO) has gained attention not only for its potential health benefits but also for its application in nanoemulsion formulation [17]. Panax ginseng C. A. Meyer, the source of ginseng, has been proven to offer various health advantages, including the potential to enhance immune responses and exhibit anti-inflammatory properties [18]. The rich content of unsaturated fatty acids in GSO has been confirmed to possess antioxidant and anti-inflammatory effects [19]. Indeed, GSO stands as a suitable candidate for synthetic emulsion; however, pertinent research on this subject remains scarce.
In this study, we utilized GSO in the oil-in-water (O/W) emulsification process for encapsulation. Briefly, gold nanoparticles were biologically synthesized using Korean ginseng root (KGR-GNP) extract. Subsequently, KGR-GNP and silydianin (bioactive compound) was formulated into a nanodroplet Korean ginseng emulsion (KGS-NE) to enhance drug delivery. Our research commenced with assessing KGS-NE treatment in Vero E6 cells infected with human coronavirus OC43 (HCoV-OC43). Subsequent investigations were carried out using two different animal models (C57BL/6 mice and Syrian hamsters) to explore the antivirus and anti-inflammatory activity of KGS-NE. Overall, this study explores the potential of KGS-NE as a promising candidate drug, providing new insights for the development of drugs against COVID-19.
Materials and methods
Materials
Dulbecco’s modified Eagle’s medium (DMEM), fetal bovine serum (FBS), and penicillin–streptomycin was purchased from GenDEPOT (Barker, TX, USA). The 1% 10 mM HEPES in 0.85% NaCl solution was sourced from Lonza, (Walkersville, MD, USA). Human coronavirus OC43 (HCoV-OC43, KBPV-VR-8) was procured from the Korea Bank for Pathogenic Viruses (Seoul, Republic of Korea). Additionally, the cDNA synthesis mix kit, qGreen Q-PCR mix kit, protease inhibitor cocktail, phosphatase inhibitor, polyvinylidene fluoride (PVDF) membranes, and enhanced chemiluminescence (ECL) solution were all purchased from Thermo Fisher Scientific (Seoul, Republic of Korea). The primers were provided by Macrogen (Seoul, Republic of Korea). Gold (III) chloride trihydrate (HAuCl4·3 H2O) was purchased from Sigma-Aldrich (St. Louis, MO, USA).
Synthesize, optimization, and physiochemical characterization of KGS-NE
Synthesis of KGS-NE
A detailed extraction of Ginseng seed oil (GSO), Korean Ginseng Root (KGR) gold nanoparticle (GNP) synthesis, and silydianin extraction was described in the supplementary file. An O/W nanoemulsion was prepared using ultrasonication (Hielscher Ultrasonics, DKSH Management Ltd., Zurich, Switzerland) [20]. In this study, GSO was utilized to synthesize KGS-NE through the O/W nanoemulsion technique. The composition of the nanoemulsion in the oily phase (GSO 8%, 4%, 6%, 8%, and 10%), silydianin (0.3 mM)) was dissolved in aqueous phase under continuous stirring at 300 rpm for 30 min. This extended stirring duration ensured thorough dispersion and solubilization of the oil phase within the aqueous medium, preventing the formation of large oil droplets or aggregates. As shown in Table S1, we optimized the hydrophilic-lipophilic balance (HLB) value by adding Tween 80 (HLB 15; surfactant) and Span 80 (HLB 4.3; co-surfactant) [21]. The combined HLB value of the surfactant mixture can be calculated using the formula:
Following the initial stirring period, the surfactant and co-surfactant were added to the solution, alongside the addition of KGR-GNP (0.5 mg/mL), and continued stirring for 1.5 h (90 min). Furthermore, KGS-NE was formed under ultrasonication at 75% amplitude within approximately 45 min following a 10 s pulse rate. The visualization of the milky white appearance of the sample confirmed the successful formation of nanoemulsion. Finally, the synthesized KGS-NE was stored at 4 °C. Moreover, the storage temperatures (4, 25, and 37 °C) of KGS-NE were checked until 6 months. For GSO nanoemulsion (NE), the oily phase at different concentrations (4%, 6%, 8%, and 10%) was optimized and the same method of preparation was used.
Characterization of synthesized KGS-NE
The physiochemical characterization of KGS-NE involved several parameters. Firstly, the morphology, elemental composition, crystallinity, and surface characteristics of the gold nanoparticles were analyzed using various techniques. Transmission electron microscopy (TEM, Tecnai G2 Spirit, FEI Company, USA.) coupled with negative staining (Nanoprobes, Yaphank, NY, USA) was employed for morphological observation, elemental mapping, selected area electron diffraction (SAED), and energy-dispersive X-ray spectrometry (EDX) analysis. Purified nanoparticles dispersed in water were deposited onto carbon-coated copper grids, dried at room temperature, and then transferred to the microscope for TEM analysis. The size, zeta potential, and polydispersity index (PDI) of the nanoparticles were determined using a dynamic light scattering (DLS) particle analyzer (Otsuka Electronics, Shiga, Japan). Additionally, an enhanced dark-field microscope (DFM, Cytoviva, Inc., Auburn, USA) was utilized to identify the particles within the KGS-NE formulation. Fourier-transform infrared (FT-IR) spectroscopy (Perkin Elmer Inc., Waltham, MA, USA) was employed to characterize the functional groups present on the surface of the KGS-NE system.
Antiviral activity of KGS-NE in HCoV-OC43- infected Vero E6 cells
Cell line and cell viability
The Vero E6 cells, originating from the African green monkey kidney (ATCC® CRL-1586), were grown in DMEM. The cell culture medium comprised 10% fetal bovine serum (FBS), 1% 10 mM HEPES in 0.85% NaCl, and 100 U/mL penicillin–100 μg/mL streptomycin. These cells were maintained at 37 °C with 5% CO2. For the experiments, Vero E6 cells were seeded at 4 × 104 cells per well in 96-well plates and incubated for 24 h. Then, KGS-NE (0.625 to 40 μg/mL), KGR-GNP (0.3 to 0.6 μg/mL), silydianin (0.1 to 0.4 mM), and GSO-NE (0.625 to 10 μg/mL) was introduced at various concentrations, and the cells were further incubated for 48 h at 37 °C. Following this incubation period, each well received 10 μL of MTT solution and underwent a subsequent 3 h incubation at 37 °C. Finally, 100 μL of DMSO was added to each well, and the cell viability was assessed by measuring the absorbance at 595 nm. For RAW 264.7 cells (Korean Cell Line Bank, Seoul, Republic of Korea), DMEM supplemented with 10% FBS (GenDEPOT, San Antonio, TX, USA) and 1% penicillin–streptomycin (P/S; GenDEPOT) was used. Cells were maintained in a humidified incubator at 37°C with 5% CO2 and 95% air. To assess cytotoxicity, RAW 264.7 cells were plated in 96-well plates at a density of 1 × 104 cells per well (SPL Life Sciences, Pocheon, Republic of Korea) and allowed to stabilize for 24 h. KGS-NE, dissolved in serum-free DMEM, was then applied to the cells at various doses, and they were incubated for an additional 24 h. Cytotoxicity was evaluated using the 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT; Thermo Fisher Scientific) assay.
Inhibitory effect of KGS-NE against HCoV-OC43 infected Vero E6 cells
Vero E6 cells were seeded at a density of 1 × 106 cells per well in 6-well plates (Corning®) and then incubated overnight at 37 °C with 5% CO2 in an incubator. Subsequently, the cells were rinsed twice with PBS and exposed to HCoV-OC43 at an infectivity level of 0.02 multiplicities (MOI) for 2 h. Throughout this period, the plates were manually agitated every 15–20 min to ensure the uniform and effective spread of the inoculum. Following adsorption, the cells were treated with various concentrations of KGS-NE. The supernatants and cells were then collected 48 h post-infection.
Transcriptomic analysis—RNA sequencing
The HCoV-OC43 infected Vero E6 cells were exposed to KGS-NE. The RNA-Seq library construction utilized total RNA, where fragmented double-strand cDNA was synthesized following the manufacturer's guidelines, employing the TruSeq Stranded mRNA Library Prep Kit (Illumina, San Diego). For an in-depth comprehension of the RNA sequencing (RNA-Seq) analysis, please refer to the detailed procedures outlined in Supplementary data.
Antiviral activity of KGS-NE using in vivo models
Animal ethics and biosafety statement
Eight-week-old male C57BL/6 mice weighing between 20–22 g was obtained from Narabiotec Co., Ltd. (Pyeongtaek, Republic of Korea). Male Syrian hamsters aged 8 weeks and weighing between 90–130 g were obtained from The Nippon Institute for Biological Science (Ome, Japan). The animals were housed in a room with a 12-h light/dark cycle (lights on 08:30–20:30), temperature of 23 ± 2 °C, and relative humidity of 54 ± 15%. They were provided food and water ad libitum, and the environmental conditions, including temperature, humidity, ventilation, and lighting, were monitored regularly during the breeding period. The experimental procedures using C57BL/6 mice and Syrian hamsters were approved by the Institutional Animal Care and Use Committee (IACUC) of Kyung Hee University (KHSASP-22-135) and IACUC of Chonbuk National University Hospital (Jeonju-si, Jeollabuk-do, South Korea), respectively. Polycarbonate breeding boxes, mats, and water bottles were used and changed weekly. Randomization and data management were performed in a blinded manner.
RBD protein-induced acute lung inflammation in C57BL/6 Mice
To determine effects of KGS-NE on acute lung inflammation induced by RBD, C57BL/6 male mice were randomly assigned to five groups: (1) Sham (saline, i.v. + saline, p.o); (2) SARS-CoV-2 RBD (RBD 200 μg/mL, i.v. + saline, p.o); (3) KGS-NE 10 (RBD 200 μg/mL, i.v. + KGS-NE 10 mg/kg, p.o); (4) KGS-NE 20 (RBD 200 μg/mL, i.v. + KGS-NE 20 mg/kg, p.o); and (5) KGS-NE 40 (RBD 200 μg/mL, i.v. + KGS-NE 40 mg/kg, p.o). The mice were orally administered control saline or KGS-NE once daily (10, 20, or 40 mg/kg) for 6 days. RBD (200 μg/mL per mouse; Catalog: SPD-C52H3; ACRO Biosystems, Newark, DE, USA) or an equivalent control saline was administered 30 min before the third KGS-NE administration. RBD protein with a His Tag is expressed in human 293 cells. It contains AA Arg 319 – Lys 537 (Accession: QHD43416.1). Its purity is > 95% as determined by SDS-PAGE and > 90% as determined by SEC-MALS (Catalog: SPD-C52H3). After RBD treatment for 3 days (24 h after the fifth KGS-NE administration), both lungs were examined to further assess the severity of acute lung inflammation. In particular, the mice were perfused with saline, the left lung was fixed via immersion in a 4% paraformaldehyde solution containing PBS for histopathological/ immunohistochemical analyses, and the right lung was fixed promptly using liquid nitrogen for western blot analysis.
SARS-CoV-2 infection in Syrian hamster
SARS-CoV-2 (NCCP No. 43330) was obtained from the National Pathogen Resources Bank and quantified in Vero E6 cells. Subsequently, the Syrian hamsters were infected with 105 plaque-forming units of the virus (100 µL) in a virus infection study. The study was conducted in a specialized ABSL-3 facility at Jeonbuk National University’s Acquisition Common Infectious Disease Research Institute. Intranasal inoculation of SARS-CoV-2 was performed to infect the hamsters in all groups (n = 7) except the Sham group. Following the SARS-CoV-2 infection, oral treatment with KGS-NE (at low: 3 mg/kg, medium: 6 mg/kg, and high: 9 mg/kg doses) was administered up to 4- day and 7-day post-infection (dpi). During the treatment phase, every hamster was examined daily to monitor for signs of mortality and to measure the body weight. By the guidelines for the use of animals, euthanasia was performed on any animals that experienced a reduction in body weight exceeding 20% throughout 72 h. Hamsters were euthanized following treatment 4 and 7 dpi, respectively. The lungs of the hamster were separated, weighed, and inspected with the naked eye. Meanwhile, the extracted left and right lobes of the lungs were set in 10% formalin for histopathological studies and frozen at -70 °C for biochemical studies.
Experimental design for in vivo non-toxicity of KGS-NE
The toxicological evaluation of KGS-NE was performed as described previously [22, 23]. C57BL/6 mice (n = 5 per group) were administered KGS-NE orally for 14 days at doses of 10, 20, 40, and 80 mg/kg. The body weight of mice was measured throughout the experiment. Mice were anesthetized by inhalation of isoflurane (1.5–3.0%) using veterinary anesthesia and monitoring equipment (SurgiVet, Waukesha, Wi, USA). The blood was collected via cardiac puncture. And the left lobe of the liver was cut into 0.3–0.5 cm thick slices and immersed in a 4% paraformaldehyde solution in 0.1 M phosphate buffered saline (pH 7.4) for histopathological assay.
Evaluation of gene expression from acute inflammatory response
RNA was extracted from homogenized lung tissues using the TRIzol reagent kit (Invitrogen, Carlsbad, CA, USA). The total RNA was reverse-transcribed into cDNA using the AmfiRivert cDNA Synthesis Platinum Enzyme Mix (GenDEPOT). qRT-PCR was performed using an AmfiSure qGreen Q-PCR Master Mix (GenDEPOT). The reaction was conducted using a Rotor-Gene Q real-time PCR detection system (Qiagen, Hilden, Germany) with SYBR Premix Ex TaqTM II (TaKaRa Bio Inc., Shiga, Japan). The gene-specific primer sequences used in this study are listed in Table S2. Target gene expression levels were calculated and normalized against the expression level of the endogenous control gene (GAPPH).
Histopathological changes and immunofluorescence analysis
To observe histopathological changes, the lung tissues were dissected and fixed in paraffin blocks for each section. Lung tissue sections were deparaffinization in xylene and subsequent rehydration through graded ethanol solutions. For Hematoxylin and Eosin (HE) staining, sections were treated with hematoxylin for 5 min, followed by a 1–2 min eosin counterstain. Post-staining, sections underwent dehydration in ascending alcohol concentrations and clearing in xylene before mounting. For immunofluorescence (IF), antigen retrieval was performed using a citrate buffer, followed by blocking with 3% hydrogen peroxide. Subsequently, sections were incubated overnight at 4 °C with primary antibodies targeting specific proteins. Secondary antibodies were applied, followed by development using DAB substrate. Lastly, sections were counterstained with hematoxylin, dehydrated, and cover-slipped for microscopic analysis.
Biochemical analysis of the serum
Serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), and lactate dehydrogenase (LDH) were quantified using enzymatic or ultraviolet assays with specific detection kits (Roche, Basel, Switzerland). The measurements were conducted following the manufacturer's instructions on a Cobas 8,000 modular analyzer (Roche), based on a protocol described previously [24,25,26,27].
Immunoblotting
Immunoblotting assay was prepared based on a previously described protocol [22, 23]. Briefly, the lung tissues were homogenized using a tissue lysis buffer comprising 10 mM Tris–Cl (pH 7.4), 0.5 mM ethylene-diamine-tetra acetic acid, 0.25 M sucrose, and a protease inhibitor mixture using a bullet blender tissue homogenizer (Next Advance, Inc., Troy, NY, USA). For the western blot assay, proteins were transferred to polyvinylidene difluoride membranes, which were then obstructed. The membranes were incubated with primary antibodies (1:2,000, Cell Signaling Technology) and horseradish peroxidase-conjugated secondary antibodies (1:500; Vector Laboratories, Newark, CA, USA). Blot signals were detected using an enhanced chemiluminescence kit (Merck KGaA). All western blot analyses were performed in triplicate and repeated thrice independently, and the results obtained were similar. The protein band density was measured using the ImageJ software.
Statistical analysis
All experiments were conducted in triplicate and the data were presented as the mean ± standard deviation. Statistical analysis was performed using the student’s t-test for comparisons between groups, with significance considered at *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001.
Results
Fatty acid composition of GSO
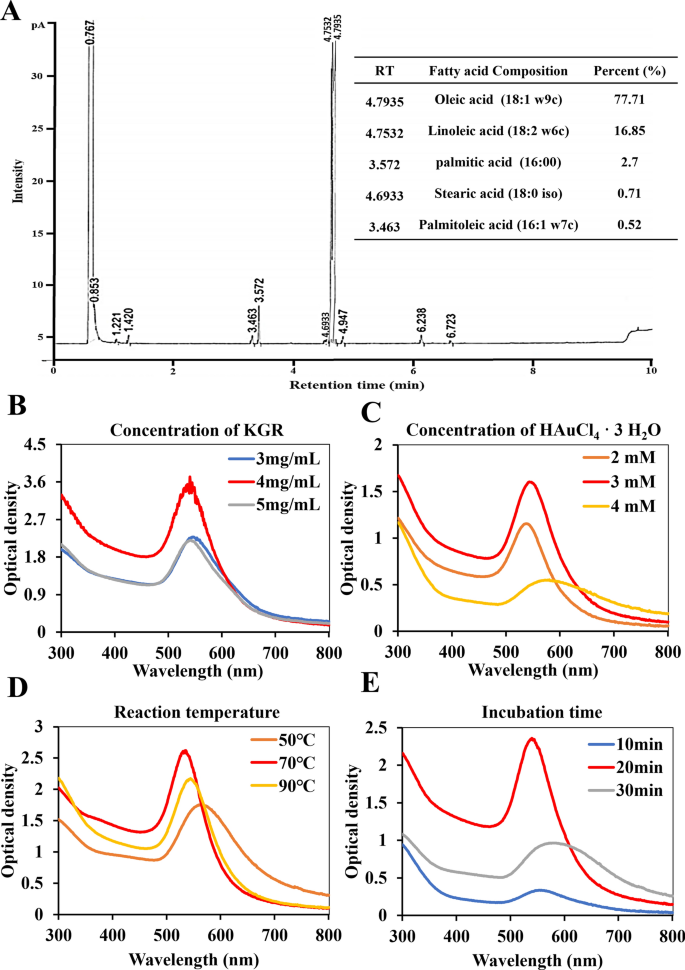
In our study, we initially analyzed the fatty acid composition of the extracted GSO using GC analysis to identify the specific types of organic compounds present. As illustrated in Fig. 1A, the principal compounds found within GSO include Oleic acid, Linoleic acid, Palmitic acid, Stearic acid, and Palmitoleic acid. Among the organic compounds in GSO, oleic acid constitutes a predominant portion at 77.71%. The second most abundant compound is linoleic acid, constituting 16.85% of the composition. In our results, minor constituents of saturated fatty acids, including Palmitic acid (2.7%) and Stearic acid (0.71%), are present in GSO. Despite the potential impact on cholesterol levels with excessive intake, GSO is generally considered safe for consumption due to the relatively low amounts present. Additionally, GSO contains a very small amount of palmitoleic acid (0.52%). Based on these findings, we found that the extracted GSO was rich in unsaturated fatty acids.
Fatty acid analysis and synthesis of KGR-GNP: A Ginseng seed oil (GSO) fatty acid composition was identified through GC analysis. The GSO contains oleic acid at 77.71%, linoleic acid at 16.85%, palmitic acid at 2.7%, stearic acid at 0.71%, and palmitoleic acid at 0.52%. B–E The optimization process for KGR-GNP synthesis is presented with variations in KGR concentration (3 to 5 mg/mL), Au concentration (2 to 4 mM), temperatures (50 to 90 °C), and incubation time (10 to 30 min)
Optimization, synthesis and physiochemical characterization of KGS-NE
Optimization of KGR-GNP
KGR-GNP was synthesized using the bio-reduction method outlined in the supplementary experimental section. Briefly, KGR was utilized as a reducing agent, and the concentrations of 4 mg/mL for KGR and 3 mM of HAuCl4·3H2O, at 70 °C for 20 min, were optimized to achieve the formation of KGR-GNP. The optimal results for the synthesis of KGR-GNP are presented in Fig. 1B-E and Table S3. As shown in Fig. 2A, the UV–Vis spectroscopy shows the synthesized KGR-GNP absorbance peak at 547 nm, which was confirmed using TEM imaging as shown in Fig. 2B.
Physicochemical characterization of KGS-NE. A The final optimized conditions for synthesizing KGR-GNP were as follows: KGR (4 mg/mL), Au (3 mM), Temperature (70 °C), and incubation time (20 min), with absorbance measured at λ max 547 nm. B Transmission electron microscope (TEM) image of KGR-GNP. C TEM image highlighting KGR-GNP (red arrow) encapsulated by KGS-NE (orange arrow). D Energy-dispersive X-ray (EDX) spectrum confirming the presence of Au in KGS-NE. E Enhanced darkfield microscope (EFM) depicting KGR-GNP inside the KGS-NE through particle reflection. F Selected area diffraction (SAED) displays the crystalline structure of KGS-NE at (111), (200), (220), and (311). G Fourier-transform infrared (FT-IR) spectrum-derived infrared absorption spectrum for confirming the functional groups of KGS-NE
Encapsulation of nanoparticle using GSO
As shown in Figure S1, the optimized GSO at different ratios demonstrated that the 8% ratio had the lowest zeta potential, indicating the highest stability at approximately − 42.54 mV. Consequently, we deliberately chose a 4:2 ratio of Tween 80 and Span 80 to achieve a targeted HLB value of 11.43 for the surfactant blend, which is within the desired range for O/W nanoemulsion [28]. Moreover, the loading efficacy of silydianin into KGS-NE was 94.3 ± 2.6%. The encapsulation content was high, above 90%, as expected in nanoemulsion systems, owing to the hydrophobic nature of silydianin. Some studies have reported that the encapsulation value decreases as the drug concentration increases, suggesting saturation of the system [29,30,31]. The presence of the surface modification monolayer was shown in the TEM image (Fig. 2C), indicating that the KGR-GNP was also successfully encapsulated by the GSO. Nanoemulsions encapsulated were denoted as KGS-NE. Various techniques were employed to confirm the encapsulation of nanoparticles into KGS-NE. Initially, the EDX spectrum, SAED pattern, and EDX were utilized to identify the presence of nanoparticles. We observed the highest Au element peak at 2.1 keV with multiple points and the appearance of a Cu peak at 8 keV was attributed to the copper grid utilized in the EDX analysis (Fig. 2D) [32]. Additionally, the DFM image (Fig. 2E) revealed particle reflections (indicated by red arrows) and the SAED pattern (Fig. 2F) shows crystallographic structures (111, 200, 220, and 311), providing further confirmation of the presence of nanoparticles [33]. FT-IR spectrometry was employed to analyze the presence of functional groups in the KGS-NE (Fig. 2G). Primary peaks were observed at 2922.09 cm−1, which corresponded to alkene C–H stretching. Meanwhile, peaks observed at two different wavelengths, i.e., 1740.24 cm−1, indicated the presence of aldehyde C=O stretching. Additionally, peaks were observed at 1098.07 cm−1, suggesting the presence of C–O stretching in the secondary alcohol.
Stability analysis
Figure 3A presents the Z-average size ranges of KGS-NE including number, volume, and intensity distribution at 202.7 nm, 87.6 nm, and 62.5 nm. The functionalization of KGS-NE showed that the particle size was 153.7 nm, PDI value of 0.25. Moreover, the zeta potential (Fig. 3B) of the KGS-NE was − 44.78 mV, indicating that the KGS-NE is stable. We observed the changes in the synthesized KGS-NE stored at various temperatures over 6 months. As shown in Fig. 3C and D, our findings indicate that the size and stability of KGS-NE remains high at 4 °C for up to 6 months compared to storage at other temperatures. Since KGS-NE is intended for oral administration, it is essential to demonstrate its stability in gastrointestinal fluids. The stability of KGS-NE was evaluated over time in simulated gastric fluid (SGF, composed of 0.2% w/v NaCl in 0.7% v/v HCl, pH 1.2) and simulated intestinal fluid (SIF, consisting of 0.05 M potassium dihydrogen phosphate and 0.02 M sodium hydroxide, pH 7.0). The results indicated that KGS-NE remained stable in both media, with no significant change in particle size observed (Figure S2). These results show that a stable KGS-NE was successfully synthesized as an O/W nanoemulsion with higher stability.
KGS-NE inhibits HCoV-OC43 infection: insights from cell viability, RNA sequencing, and pathway analysis
HCoV-OC43, belonging to the identical viral genus as SARS-CoV and SARS-CoV-2, demonstrates comparable symptoms to those elicited by SARS-CoV-2 [34]. We preliminarily tested the cytotoxicity and viral inhibition effects of KGR-GNP, silydianin, GSO-NE, and KGS-NE against HCoV-OC43. As shown in Figure S3, the non-toxic concentrations of KGR-GNP, silydianin, and GSO-NE were chosen. However, KGR-GNP, silydianin, and GSO-NE did not show better activity than KGS-NE in the non-toxic concentration. Therefore, in further experiments, we focused on studying the antiviral effect of KGS-NE. In a further study, we first examined the antiviral activity of KGS-NE in Vero-E6 cells infected with HCoV-OC43 to explore its efficacy against the virus. In Fig. 4A, a cell viability assay was performed on Vero E6 cells. The MTT assay results revealed that KGS-NE did not show significant cytotoxicity until the concentration reached 10 μg/mL, and the IC50 value of KGS-NE in Vero E6 cells was determined to be 24.92 μg/mL (Fig. 4B). Moreover, as shown in Fig. 4C, different concentrations of KGS-NE were used to quantitatively analyze its effect on HCoV-OC43 N gene production. The results demonstrated that KGS-NE treatments dose-dependently suppressed HCoV-OC43 replication, with viral RNA levels reduced by 98% at 0.5 μg/mL. This result indicated that KGS-NE exhibits antiviral effects in HCoV-OC43-infected Vero E6 cells. Subsequently, we conducted an RNA sequencing analysis of the differentially expressed genes (DEGs) involved in the Vero E6 cells. This analysis aimed to explore the potential of KGS-NE on antiviral and anti-inflammatory effects and its underlying mechanism. As shown in Fig. 4D, treatment with KGS-NE resulted in the DEGs of 145 down-regulated and 178 up-regulated significant genes, as compared to the HCoV-OC43 infection group. The DEGs data was used to show the distribution of genes that were differentially expressed with a fold change of greater than 1.2 or less than 0.8, and a p-value less than 0.05.
Effect of KGS-NE treatment on Vero E6 cells infected by human coronavirus OC43 (HCoV-OC43). A, B Cell viability in Vero E6 cells treated with KGS-NE, including the determination of IC50 value. C RNA levels in HCoV-OC43-infected Vero E6 cells treated with KGS-NE. D Visualization of up-and down-regulated Differential Gene Expressions (DEGs) using a volcano plot. E Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis indicating significant signaling pathways. F Heatmap representation of DEGs involved in the ABC transporters signaling pathway. G Gene Ontology (GO) analysis of biological processes (BP), cellular component (CC), and molecular interactions (MF)
The Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment bubble plots were utilized to summarize the correlation between significant pathways. Figure 4E and Table S4 provided the KEGG mapping of significant genes and their corresponding fold enrichment values. Our study identified several significant signaling pathways, among which ABC transporters exhibited the highest enrichment score, indicating that the ABC transporter's signaling pathway might serve as the primary regulator. Moreover, as shown in Fig. 4F, the genes associated with the ABC transporters are visualized through a heatmap. This heatmap illustrates the regulation of ABC genes, including their subfamilies, under the influence of KGS-NE treatment and HCoV-OC43 infection. The result shows that the ABC transporters family gene regulations were reversed by KGS-NE treatment. Notably, the ABC transporters subfamily F had significantly opposite regulation among these groups. Therefore, the observed differential regulation of ABCF2 and ABCF3 genes could be indicative of the critical function between the host and the virus. The downregulation after treatment suggests a potential positive response to the intervention by KGS-NE.
Additionally, comprehensive Gene Ontology (GO) enrichment analyses were performed to evaluate the biological functions of all identified DEGs. The GO analysis, encompassing Biological Processes (BP), Cellular Component (CC), and Molecular Function (MF), is presented in Fig. 4G. Within BP, the most significantly enriched genes were associated with catabolic and metabolic pathways. In CC, peroxisomes and microbodies exhibited a similar number of genes with notable enrichment scores. MF, ATPase-coupled transmembrane, Primary active transmembrane, and ATPase activity demonstrated the highest significant enrichment scores. Notably, when comparing BP, CC, and MF the MF shows the highest number of enrichment scores. The GO fold enrichment values of signaling pathways were presented in Tables S5, S6, and S7. Collectively, the Gene Ontology (GO) results provide a comprehensive depiction of the molecular intricacies influenced by KGS-NE treatment including a substantial impact on cellular processes related to energy metabolism and energy-dependent transmembrane transport and ATP hydrolysis.
KGS-NE attenuates lung tissue damage in SARS-CoV-2 spike RBD protein induction in mice
Using SARS-CoV-2 spike RBD protein in mice allows for immune response studies and specific investigations without causing a full COVID-19 infection in mice, as they are not naturally susceptible to SARS-CoV-2. This approach aids in understanding immune responses, developing vaccines, and exploring virus-host cell interactions. After confirming the antiviral efficacy of KGS-NE in Vero E6 cells, additional validation of its effects was evaluated using the SARS-CoV-2 spike RBD protein. To explore the in vivo immune response potential of KGS-NE, mice were orally administered KGS-NE for two days (pre-infection). Subsequently, on the third day, after a 5 h interval from the oral administration of KGS-NE, mice were intratracheally inoculated with SARS-CoV-2 spike RBD. As depicted in Fig. 5A, the treatment regimen was maintained for the next four days (post-infection), totaling six days of the treatment. Following KGS-NE treatment, the severity of acute lung injury was evaluated in the mice at 7 dpi. Histological analysis (Fig. 5B) of lung tissues via H&E staining revealed that RBD protein led to the infiltration of inflammatory cells and thickening of alveolar walls, indicating severe damage to lung tissues. Moreover, the inflammatory score indicates that oral administration of KGS-NE was able to inhibit these conditions and mitigate the adverse effects of RBD protein in a dose-dependent manner. The observed recovery was approximately 56% at the highest dose of 40 mg/kg. The results suggest that administration with KGS-NE alleviates lung injury induced by the RBD protein.
Effect of KGS-NE in SARS-CoV-2 spike receptor binding domain (RBD) protein-induced C57BL/6 mice. A Schematic representation of mice treatment groups. Mice were categorized into five groups: Group 1: Sham group; Group 2: RBD spike protein-induced group; Group 3: RBD spike protein-induced with KGS-NE (10 mg/kg) treatment group; Group 4: RBD spike protein-induced with KGS-NE (20 mg/kg) treatment group; and Group 5: RBD spike protein-induced with KGS-NE (40 mg/kg) treatment group. B Histopathology staining was performed to determine the pathology in the lungs, and the inflammatory score was calculated. C IF staining of ACE2, CD68, and Iba-1 where the intensity is shown in the bar graph. Crosshatch marks indicate significant differences between sham and SARS-CoV-2 RBD, and asterisks indicate significant differences between SARS-CoV-2 RBD and each group. *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001
Angiotensin-converting enzyme (ACE) is a central component of the renin-angiotensin system, crucial for blood pressure and fluid homeostasis. In the context of SARS-CoV-2, the RBD protein binds to ACE2 (Angiotensin-Converting Enzyme 2) as the primary mechanism for cellular entry, contributing to the development of lung injury [35]. Therefore, we investigated whether KGS-NE activates the immune response by affecting the binding of RBD protein to ACE2. Based on the IF staining results shown in Fig. 5C, the RBD protein enhanced the levels of ACE2 expression. In contrast, KGS-NE administration suppressed ACE2 expression by 72%, even at a low concentration of 10 mg/kg. In addition, Ionized calcium-binding adapter molecule 1 (Iba1) and Cluster of Differentiation 68 (CD68) both are commonly used markers in IF to identify the presence of macrophages, which is vital to the immune response of the lungs. Our IF staining results for Iba-1 and CD68 show that the expression was higher in the group treated with RBD protein than in the sham group indicated. After the administration of KGS-NE, it suppressed the Iba-1 and CD68 expression. These results suggest that KGS-NE could prevent acute lung injury caused by the RBD protein through the modulation of ACE2, Iba-1, and CD68. This could indicate a potential mitigation of an overactive or dysregulated immune response, thereby reducing the risk of excessive inflammation or tissue damage.
Moreover, the expression of ACE2, Iba-1, and CD68 was further confirmed through immunoblotting. As depicted in Fig. 6A and B, RBD induction dramatically upregulated the expression of ACE2, Iba-1, and CD68 proteins. Conversely, KGS-NE administration significantly inhibited this upregulation. These collective results strengthen the impact of KGS-NE on immune regulators (ACE2, Iba-1, and CD68), highlighting its potential in modulating immune responses linked to RBD-induced protein expression. In addition to the observed impact on ACE2, Iba-1, and CD68 expression, the pro-inflammatory cytokines (IL-6 and IL-1β) were also evaluated. This analysis could enhance our understanding of KGS-NE immunomodulatory effects in response to RBD induction. Our results show that these proteins were significantly overexpressed by RBD induction, whereas treating with KGS-NE suppressed these expressions. Notably, IL-1β protein expression was suppressed by approximately 89% at the highest dose compared to the infection group. Nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) serves as a crucial transcriptional activator of cytokines implicated in the innate immune response, such as IL-6 and IL-1β. Beyond its prominent role in innate immunity, NF-κB also plays significant functions in the adaptive immune system. In this study, we assessed the expression of NF-κB protein upon RBD induction. The results indicate a significant upregulation of NF-κB by RBD induction, and KGS-NE exhibited a dose-dependent suppression of its expression. These findings support KGS-NE diverse immunomodulatory impact on key cytokines in the immune response.
Effects of KGS-NE on inflammatory regulators. A Demonstrates that KGS-NE treatment suppressed ACE2, Iba-1, CD68, IL-6, p-NF-κB/NF-κB through protein expression. B A bar graph represents the protein expression analyzed using Image J. Crosshatch marks indicate significant differences between sham and SARS-CoV-2 RBD, while asterisks indicate significant differences between SARS-CoV-2 RBD and each group. *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001
KGS-NE modulates antiviral and anti-inflammatory effects in SARS-CoV-2-infected Syrian hamsters
Syrian hamster was chosen as the experimental animal model to evaluate the feasibility of KGS-NE to inhibit SARS-CoV-2. The Syrian hamsters are small mammals that have been widely used as a model for infection with respiratory viruses, including SARS-CoV-2, influenza viruses, and adenoviruses. In this study, we conducted an assessment to investigate the impact of KGS-NE on SARS-CoV-2-induced pneumonia. The assessment was conducted employing a Syrian hamster model subjected to intranasal infection with SARS-CoV-2, followed by therapeutic intervention utilizing varying dosage levels of KGS-NE. KGS-NE was orally administered (1–6 dpi) after SARS-CoV-2 infection, as shown in Fig. 7A. The weight loss and virus replication number of hamsters were assessed at 4 dpi and 7 dpi, respectively. As depicted in Fig. 7B and C, hamsters infected with SARS-CoV-2 exhibited a decrease in body weight. However, the dose-dependent administration of KGS-NE could alleviate the effects of SARS-CoV-2 infection. Further, the lungs of the hamsters were dissected to examine the effect of KGS-NE treatment against SARS-CoV-2 infection.
Effect of KGS-NE in SARS-CoV-2 infected Syrian hamsters. A Schematic representation of Syrian hamster treatment groups. (B, C Body weight changes in grams and percentage after infecting SARS-CoV-2 and KGS-NE administration. D, E RT-PCR was used to estimate the viral load of RdRp and E gene. Crosshatch marks indicate significant differences between sham and SARS-CoV-2 RBD, while asterisks indicate significant differences between SARS-CoV-2 RBD and each group. *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001
The RNA-dependent RNA polymerase (RdRp) and envelope (E) genes are essential targets for the detection and diagnosis of SARS-CoV-2 infections [36]. Subsequently, we evaluated the RNA copy number of the SARS-CoV-2 specific sequence while targeting the RdRp and E genes to determine whether KGS-NE can prevent the replication of SARS-CoV-2 in lung tissue. As shown in Fig. 7D and E, the expression of RdRp and E genes increased significantly in the SARS-CoV-2 infection, whereas the administration of KGS-NE slightly suppressed the expression of RdRp and E genes.
As shown in Fig. 8A, inflammation was observed in the lungs of SARS-CoV-2-infected hamsters, and these abnormalities were suppressed by administration of KGS-NE. Specifically, lung congestion and swelling escalated over time in SARS-CoV-2-infected hamsters. In contrast, the KGS-NE group demonstrated the ability to reduce this congestion and swelling in a dose- and time-dependent manner. In addition, as shown in Fig. 8B, H&E staining was performed on the lung tissue of hamsters to evaluate the pathological changes in lung tissue caused by SARS-CoV-2 infection. Pathological lung tissue inflammation (red arrow), such as alveolar damage, vascular changes, fibrosis, and morphological disruption, was observed in SARS-CoV-2 infection and was dose-dependently attenuated by KGS-NE administration.
Effect of KGS-NE on lung morphological changes in Syrian hamsters infected with SARS-CoV-2. A Morphology of the dissected lungs in 4 and 7 dpi along with the weight. B Histopathology (H&E) staining performed to assess lung pathology and calculate the inflammatory score. Crosshatch marks indicate significant differences between sham and SARS-CoV-2 infection, and asterisks indicate significant differences between SARS-CoV-2 infection and each group. *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001
To substantiate the inhibitory effects of KGS-NE on the inflammatory response induced by SARS-CoV-2, a qRT-PCR examination was conducted to scrutinize the regulatory impact of KGS-NE on the gene expression of pro-inflammatory cytokines, including NF-κB, IL-1β, IL-6, MCP-1, and TNF-α (Fig. 9). The results unveiled an elevation in the levels of pro-inflammatory cytokines such as NF-κB, IL-1β, IL-6, MCP-1, and TNF-α in hamsters infected with SARS-CoV-2, indicative of an augmented immune response and an inflammatory cascade initiated by viral infection. The intrusion of the coronavirus triggers the activation of the host immune system, prompting cellular synthesis of these pro-inflammatory factors as a defensive measure against infection. In contrast, administration of KGS-NE demonstrated a capacity to down-regulate the gene expression associated with pro-inflammatory cytokines, signifying its potential to attenuate the heightened inflammatory response induced by viral infection. Furthermore, KGS-NE exhibited a substantial reduction in the gene expression of ACE2 in hamster lung tissue. At 4 days post-infection (dpi), there was a 46% reduction, and at 7 dpi, there was a 58% reduction, demonstrating a time-dependent and dose-dependent manner. This observation suggests that KGS-NE may attenuate cellular susceptibility to viruses by diminishing ACE2 gene expression, thereby decelerating the process of virus invasion into host cells. Furthermore, as shown in Figure S4, KEGG pathway analysis identified significant expression of ABC transporter genes, particularly ABCF2 and ABCF3, which were confirmed through qRT-PCR analysis. In summary, these findings collectively endorse the potential of KGS-NE to modulate immune responses and alleviate pulmonary inflammation in hamsters during SARS-CoV-2 infection.
Effect of KGS-NE on lung inflammation in Syrian hamsters infected with SARS-CoV-2. A–F mRNA expression of inflammatory cytokines (IL-6, IL-1β, TNF-α and MCP1), and suppression of ACE2 and NF-κB in KGS-NE administrated group. Crosshatch marks indicate significant differences between sham and SARS-CoV-2 infection, and asterisks indicate significant differences between SARS-CoV-2 infection and each group. *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001
In vivo toxicity assessment of KGS-NE administration
The toxicity assessment of drugs in the serum and liver is critical because these organs participate in drug metabolism and elimination [37]. In this study, the toxicity of KGS-NE was investigated via oral administrations of different concentrations (10–80 mg/kg) to C57BL/6 mice aged eight weeks for 14 days (Fig. 10A). The effect of KGS-NE treatment on the body weight of the mice was evaluated, and the results (shown in Fig. 10B) indicate no significant change in the body weight. Liver histology was assessed via H&E staining (Fig. 10C). Normal liver tissue typically displays cords of hepatocytes with a central vein and sinusoids, and hepatocyte nuclei are typically round or oval with prominent nucleoli. H&E staining showed hepatocyte swelling, necrosis, and inflammation, suggesting liver disease or toxic injury. However, in the present study, KGS-NE (80 mg/kg) did not induce any of these changes, indicating that its non-toxicity to the liver. ALT and AST levels were quantified to evaluate liver function and identify liver injury, whereas ALP and LDH levels were investigated as potential indicators of liver disease. The results are presented in Fig. 10D. The enzyme activities were similar in the non-treatment group, indicating that prolonged KGS-NE administration did not induce significant toxicity. In general, these results suggest that the administration of KGS-NE does not affect liver damage. Moreover, to address concerns about the immune response, we assessed the proportion of immune cells in mice. Specifically, we analyzed the effect of KGS-NE on RAW 264.7 macrophage cells, focusing on cell proliferation. As shown in Figure S5, the results showed no significant changes in cell proliferation after treatment with KGS-NE (40 mg/kg), indicating that KGS-NE does not have toxic effects on immune cells. Overall, these findings demonstrate that KGS-NE is safe with respect to liver function and immune cell health.
In vivo toxicity evaluation of KGS-NE in C57BL/6 mice. A Schematic representation of KGS-NE administration in C57BL/6 mice. B Changes in body weight during experimental period were insignificant; C Histopathological (H&E) examination of liver tissue showed no indications of damage following saPGS-NE administration. D Serum tests for liver function markers, including ALT, ALP, AST, and LDH, showed no evidence of toxicity. Crosshatch marks indicate significant differences between each group. *, # p < 0.05, **, ## p < 0.01, and ***, ### p < 0.001
Discussion
Nano-drug delivery systems are extensively used in clinical applications and offer numerous advantages [38]. In this study, we designed a nanoemulsion drug delivery system encapsulating metal nanoparticles and characterized its physicochemical properties. In addition to selecting edible GSO as the encapsulation material, we also creatively loaded the bioactive compound silydianin. Our previous research results showed that silydianin has good antiviral activity, but its poor water solubility limits its drug ability. However, the nanoemulsion method can effectively encapsulate and deliver it. The synthesized nanoemulsion also showed good antiviral effects. In the future, our research will focus more on designing smart nanoemulsion systems to achieve controlled release of drugs under specific environments such as pH, temperature, enzymes, etc. By utilization of NEs for drug delivery was based on diverse advantages over previously reported formulations. According to several reports, the formulation of NEs prepared from food-grade excipients exhibits commendable biocompatibility and safety [39]. Furthermore, NEs can be produced using homogenization methods, rendering them conducive to scalable industrial production. Studies have indicated that NEs with a size of approximately 100 nm are more easily internalized by lung epithelial cells [40]. Generally, nanoparticles with diameters ranging from approximately 20 to 200 nm exhibit enhanced performance in cellular uptake [41]. Notably, KGS-NE, with a diameter of around 20 nm, aligns with the optimal size range for efficient cellular internalization, providing a size advantage and biosafety compared to conventional inhalation suspensions.
Long-term storage stability is a critical parameter in the development of nanomaterial-based drug delivery systems [42]. Stable nanoemulsions are essential as they retain their physicochemical properties over extended periods, which is crucial for their practical application [43]. The present study demonstrates that the KGS-NE formulation exhibits robust stability over six months, particularly when stored under refrigeration at 4 °C. This finding underscores the potential of KGS-NE for various biomedical applications, given that maintaining stability under these conditions ensures consistent performance and safety. A significant challenge in the stability of nanoemulsions is lipid oxidation [44], which can lead to detrimental effects such as rancidity, nutrient degradation, and structural changes. Considering this, our formulation incorporates specific strategies aimed at mitigating oxidation. The choice of emulsifiers Tween 80 and Span 80 is pivotal. These emulsifiers form a protective barrier around lipid droplets, significantly reducing the risk of oxidative reactions [44]. The efficacy of this approach is evidenced by the sustained stability of KGS-NE observed in our study. Additionally, the storage conditions play a vital role in prolonging the shelf life of nanoemulsions. Refrigeration at 4 °C has been shown to decelerate the oxidation process, thereby preserving the integrity of the formulation. Thus, future research should focus on optimizing the nanoemulsification process to produce nanoemulsions with higher oxidative stability. Additionally, a balance should be achieved between the efficiency of novel emulsion stabilizing strategies and their cost-effectiveness and operability on a large scale.
In our in vitro study, we systematically investigated the antiviral mechanisms underlying KGS-NE's inhibitory effects against HCoV-OC43 infection. We unequivocally demonstrated the antiviral activity of KGS-NE against HCoV-OC43, thereby providing solid support for its potential therapeutic application in combating coronavirus infections. Given the taxonomic relationship between HCoV-OC43 and SARS-CoV-2 within the same virus genus [45], the broad-spectrum antiviral effects of KGS-NE suggest potential therapeutic value across various coronaviruses. Furthermore, employing RNA sequencing and pathway analysis, we delved into the intricate mechanisms of action exerted by KGS-NE. Notably, KGS-NE exhibited extensive modulation of gene expression at the cellular level, particularly impacting signal pathways associated with the ABC transporter protein family. ABC transport proteins play a direct role in the activation of immune cells and inflammatory responses [46]. They exert their influence by potentially impacting pathways such as antigen presentation, T-cell activation, and the generation of inflammatory mediators, thereby directly modulating the intensity and nature of immune responses [47]. For instance, during the antigen presentation process, ABC transport proteins assist in transporting antigens to the cell membrane, facilitating the recognition and activation of T cells [48]. This molecular-level information not only elucidates the antiviral efficacy of KGS-NE but also provides crucial insights for the prospective development of related therapeutic strategies. Subsequent GO analysis unveiled the comprehensive impact of KGS-NE treatment on cellular processes, cellular components, and molecular functions, encompassing critical biological functions such as energy metabolism and ATPase activity. This comprehensive comprehension aids in deciphering the intricate regulatory mechanisms orchestrated by KGS-NE. In conclusion, our study not only provides experimental evidence for the potential application of KGS-NE in antiviral therapeutics but also unravels the intricate molecular mechanisms underlying its multifaceted antiviral effects.
Our in vivo experiments have demonstrated a significant mitigation effect of KGS-NE on lung tissue damage induced by the SARS-CoV-2 spike (S) RBD protein. Concerning the immunomodulatory effects of KGS-NE, we observed its ability to suppress acute lung injury induced by the RBD protein through the regulation of immune modulators such as ACE2, Iba-1, and CD68. This multifaceted mechanism positions KGS-NE as an effective intervention for attenuating inflammatory responses and maintaining tissue integrity, particularly crucial in the face of challenges posed by viral variations and immune evasion [49]. It is noteworthy that current research indicates the binding capability of oleic acid found in GSO, utilized in the synthesis of KGS-NE, with the coronavirus S protein [50]. This discovery adds depth to our understanding of the mechanisms underlying KGS-NE as an antiviral agent. Further investigations can focus on elucidating the specific mechanisms of interaction between KGS-NE and the coronavirus S protein, shedding light on the impact of this binding on infection. Therefore, our study reveals that orally administered KGS-NE exhibits excellent therapeutic efficacy in treating acute lung injury induced by SARS-CoV-2 in mice. Specifically, KGS-NE effectively reduces viral copy numbers in target cells after oral administration, consequently reducing inflammation in hamster lungs. This approach significantly diminishes inflammatory cell infiltration, and pro-inflammatory cytokine secretion, and alleviates lung tissue damage. Hence, our drug delivery platform shows promise for future applications in combating novel coronaviruses and respiratory system diseases.
Our research underscores that KGS-NE is a nanoemulsion with robust biocompatibility and stability, demonstrating the ability to dose-dependently reduce ACE2 protein levels. However, despite its significant potential in infection prevention, caution is advised in its prolonged and high-dose usage due to potential side effects. Hence, a more in-depth investigation and monitoring are warranted to assess the potential risks associated with long-term KGS-NE usage, especially concerning the physiological processes related to ACE2. Intriguingly, our study indicates that KGS-NE does not impact the physiological transcriptional expression of ACE2 in hamsters. This implies that cellular ACE2 expression is not irreversibly compromised, and transcription can recover upon cessation or limitation of KGS-NE administration, providing a degree of assurance regarding the safety and reversibility of KGS-NE. Notably, during pneumonia, ACE2 expression in lung tissues was upregulated, potentially associated with increased interferon expression. This upregulation might accelerate the spread of SARS-CoV-2, forming a detrimental cycle [51]. Therefore, future research should further investigate the efficacy of combining KGS-NE with antiviral and anti-inflammatory drugs in the treatment of COVID-19, aiming for a more comprehensive and synergistic therapeutic strategy. This approach will help ensure the maximal utilization of the potential advantages of KGS-NE while minimizing potential adverse effects.
Conclusion
In this study, we demonstrated that KGS-NE, a self-assembled NE-based therapeutic agent, effectively treated COVID-19. Our findings indicate that KGS-NE successfully recovered SARS-CoV-2 viral infection in C57BL/6 mice and Syrian hamsters by inhibiting pro-inflammatory cytokines and macrophages, suppressing the expression of crucial markers of viral infection such as NF-κB and STAT3, and reducing lung inflammation. In addition, KGS-NE administration (80 mg/kg) did not cause toxicity and effectively attenuated the acute inflammatory response associated with SARS-CoV-2 infection by suppressing RdRp and E gene expression. Our results suggest that KGS-NE is a promising treatment option for SARS-CoV-2 infections. Further clinical studies are required to investigate the effects of KGS-NE on humans infected with SARS-CoV-2. In summary, further research is necessary to establish the efficacy and safety of KGS-NE as a potential treatment for SARS-CoV-2 infections in humans.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- SARS‑CoV‑2:
-
Severe acute respiratory syndrome coronavirus 2
- RBD:
-
Receptor binding domain
- ACE2:
-
Angiotensin-converting enzyme 2
- GNP:
-
Gold nanoparticles
- O/W:
-
Oil-in-water
- DFM:
-
Dark field microscope
- TEM:
-
Transmission electron microscope
- FTIR:
-
Fourier transform infrared spectroscopy
- DLS:
-
Dynamic light scattering
- EDX:
-
Elemental mapping
- HCoV-OC43:
-
Human coronavirus
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes Enrichment
- PPI:
-
Protein-protein interaction
- GO:
-
Gene ontology
- DEG:
-
Differential gene expression
- IF:
-
Immunofluorescence
- NF-κB:
-
Nuclear factor immunoglobulin kappa chain enhancer B
- IL-1β:
-
Interleukin-1β
- IL-6:
-
Interleukin-6
- MCP1:
-
Monocyte chemoattractant protein-1
- PDI:
-
Polydispersity index
- DMSO:
-
Dimethyl sulfoxide
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- LDH:
-
Lactate dehydrogenase
References
Razimoghadam M, et al. Changes in emergency department visits and mortality during the COVID-19 pandemic: a retrospective analysis of 956 hospitals. Arch Public Health. 2024;82(1):1–12.
Balogun OD, et al. Innovations in drug delivery systems: a review of the pharmacist’s role in enhancing efficacy and patient compliance. World J Adv Res Rev. 2023. https://doiorg.publicaciones.saludcastillayleon.es/10.30574/wjarr.2023.20.3.2587.
Ashour NA, et al. A systematic review of the global intervention for SARS-CoV-2 combating: from drugs repurposing to molnupiravir approval. Drug Des Dev Therapy. 2023. https://doiorg.publicaciones.saludcastillayleon.es/10.2147/DDDT.S354841.
Inagaki K, Hobbs CV. COVID-19: a pediatric update in epidemiology, management, prevention, and long-term effects. Pediatr Rev. 2023;44(5):243–54.
Ao D, et al. Strategies for the development and approval of COVID-19 vaccines and therapeutics in the post-pandemic period. Signal Transduct Target Ther. 2023;8(1):466.
Srivastav AK et al. Lipid based drug delivery systems for oral, transdermal and parenteral delivery: recent strategies for targeted delivery consistent with different clinical application. J Drug Deliv Sci Technol. 2023; 104526.85(11): 1–22.
Pathak K. Herbal nanotechnology: innovations and applications in modern medicine.Indian J Nat Products. 2023;14(10);1–10.
Huang R et al. Nano-based theranostic approaches for the infection control: current states and perspectives. Mater Chem Front. 2024.2024. 8; 9–40.
Nag S, et al. Exploring the emerging trends in the synthesis and theranostic paradigms of cerium oxide nanoparticles (CeONPs): a comprehensive review. Mater Today Chem. 2024;35: 101894.
Mehta M, et al. Lipid-based nanoparticles for drug/gene delivery: an overview of the production techniques and difficulties encountered in their industrial development. ACS Mater Au. 2023;3(6):600–19.
Gasa-Falcon A, et al. Nanostructured lipid-based delivery systems as a strategy to increase functionality of bioactive compounds. Foods. 2020;9(3):325.
Dhiman N, et al. Lipid nanoparticles as carriers for bioactive delivery. Front Chem. 2021;9: 580118.
Low LE, et al. Recent advances of characterization techniques for the formation, physical properties and stability of Pickering emulsion. Adv Coll Interface Sci. 2020;277: 102117.
Lakshmayya N, et al. Essential oils-based nano-emulsion system for food safety and preservation: current status and future prospects. Biocatal Agric Biotechnol. 2023;53: 102897.
Sambhakar S, et al. Nanoemulsion: an emerging novel technology for improving the bioavailability of drugs. Scientifica. 2023. https://doiorg.publicaciones.saludcastillayleon.es/10.1155/2023/6640103.
Nejatian M, et al. Improving the storage and oxidative stability of essential fatty acids by different encapsulation methods; a review. Int J Biol Macromol. 2024;260: 129548.
Truong V-L, Jeong W-S. Red ginseng (Panax ginseng Meyer) oil: a comprehensive review of extraction technologies, chemical composition, health benefits, molecular mechanisms, and safety. J Ginseng Res. 2022;46(2):214–24.
Feng L, et al. Structural analysis of a soluble polysaccharide GSPA-0.3 from the root of Panax ginseng CA Meyer and its adjuvant activity with mechanism investigation. Carbohydrate Polym. 2024;326: 121591.
Farag MA, Gad MZ. Omega-9 fatty acids: potential roles in inflammation and cancer management. J Genet Eng Biotechnol. 2022;20(1):1–11.
Carpenter J, Saharan VK. Ultrasonic assisted formation and stability of mustard oil in water nanoemulsion: effect of process parameters and their optimization. Ultrason Sonochem. 2017;35:422–30.
Siddique MY, et al. Formulation of gelled microemulsion for effective permeation of celecoxib across the skin barrier. ChemistrySelect. 2024;9(3): e202302841.
Kim EJ, et al. Schisandra chinensis stem ameliorates 3-nitropropionic acid-induced striatal toxicity via activation of the Nrf2 pathway and inhibition of the MAPKs and NF-kappaB pathways. Front Pharmacol. 2017;8:673.
Choi JH, et al. An oriental medicine, Hyungbangpaedok-San attenuates motor paralysis in an experimental model of multiple sclerosis by regulating the T cell response. PLoS ONE. 2015;10(10): e0138592.
Jang M, et al. Oriental medicine Kyung-Ok-Ko prevents and alleviates dehydroepiandrosterone-induced polycystic ovarian syndrome in rats. PLoS ONE. 2014;9(2): e87623.
Kim E-J, et al. Schisandra chinensis stem ameliorates 3-nitropropionic acid-induced striatal toxicity via activation of the Nrf2 pathway and inhibition of the MAPKs and NF-κB pathways. Front Pharmacol. 2017;8:673.
Wang R, et al. 8-Paradol from ginger exacerbates PINK1/Parkin mediated mitophagy to induce apoptosis in human gastric adenocarcinoma. Pharmacol Res. 2023;187: 106610.
Dhandapani S, et al. Lysine-rich polypeptide modulates forkhead box o3 and phosphoinositide 3-kinase-protein kinase B pathway to induce apoptosis in breast cancer. ACS Pharmacol Transl Sci. 2024. https://doiorg.publicaciones.saludcastillayleon.es/10.1021/acsptsci.4c00221.
Confessor MVA, et al. Olive oil nanoemulsion containing curcumin: antimicrobial agent against multidrug-resistant bacteria. Appl Microbiol Biotechnol. 2024;108(1):241.
Brouwers J, Brewster ME, Augustijns P. Supersaturating drug delivery systems: the answer to solubility-limited oral bioavailability? J Pharm Sci. 2009;98(8):2549–72.
Li Y, et al. Nanoemulsion-based delivery systems for poorly water-soluble bioactive compounds: influence of formulation parameters on polymethoxyflavone crystallization. Food Hydrocolloids. 2012;27(2):517–28.
Warren DB, et al. Using polymeric precipitation inhibitors to improve the absorption of poorly water-soluble drugs: a mechanistic basis for utility. J Drug Target. 2010;18(10):704–31.
Dhandapani S, et al. Enhanced skin anti-inflammatory and moisturizing action of gold nanoparticles produced utilizing Diospyros kaki fruit extracts. Arab J Chem. 2023;16(4): 104551.
Dhandapani S, et al. Exploring the potential anti-inflammatory effect of biosynthesized gold nanoparticles using Isodon excisus leaf tissue in human keratinocytes. Arab J Chem. 2023;16(10): 105113.
Hirahata T et al. A review of SARS-CoV-2 virology, vaccines, variants and their impact on the COVID-19 pandemic. Rev Res Med Microbiol. 2024; 10.1097.35:1–24.
Ou J, et al. V367F mutation in SARS-CoV-2 spike RBD emerging during the early transmission phase enhances viral infectivity through increased human ACE2 receptor binding affinity. J Virol. 2021;95(16):e00617-e621.
Abbasi H, et al. Real-time PCR Ct value in SARS-CoV-2 detection: RdRp or N gene? Infection. 2022;50(2):537–40.
Murphy WA, et al. Considerations for physiologically based modeling in liver disease: from nonalcoholic fatty liver (NAFL) to nonalcoholic steatohepatitis (NASH). Clin Pharmacol Ther. 2023;113(2):275–97.
Lv Y, et al. Nano-drug delivery systems based on natural products. Int J Nanomed. 2024;19:541–69.
Li G, et al. Nanoemulsion-based delivery approaches for nutraceuticals: fabrication, application, characterization, biological fate, potential toxicity and future trends. Food Funct. 2021;12(5):1933–53.
Gomes dos Reis L, et al. Delivery of pDNA to lung epithelial cells using PLGA nanoparticles formulated with a cell-penetrating peptide: understanding the intracellular fate. Drug Dev Ind Pharm. 2020;46(3):427–42.
Augustine R, et al. Cellular uptake and retention of nanoparticles: insights on particle properties and interaction with cellular components. Mater Today Commun. 2020;25: 101692.
Cheng X, Xie Q, Sun Y. Advances in nanomaterial-based targeted drug delivery systems. Front Bioeng Biotechnol. 2023;11:1177151.
Mushtaq A, et al. Recent insights into nanoemulsions: their preparation, properties and applications. Food Chem X. 2023;18: 100684.
Villeneuve P, et al. Lipid oxidation in emulsions and bulk oils: a review of the importance of micelles. Crit Rev Food Sci Nutr. 2023;63(20):4687–727.
You C, et al. The publicly-accessible RNA barcode segments based on the genetic tests of complete genome sequences for SARS-CoV-2 identification from HCoVs and SARSr-CoV-2 lineages. Virol Sinica. 2024. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.virs.2024.01.006.
Fan J, et al. ABC transporters affects tumor immune microenvironment to regulate cancer immunotherapy and multidrug resistance. Drug Resist Updates. 2023;66: 100905.
Thurm C, Schraven B, Kahlfuss S. ABC transporters in T cell-mediated physiological and pathological immune responses. Int J Mol Sci. 2021;22(17):9186.
Guo W, Qiao T, Li T. The role of stem cells in small-cell lung cancer: evidence from chemoresistance to immunotherapy. Semin Cancer Biol. 2022. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.semcancer.2022.11.006.
Vanderheiden A, Klein RS. Neuroinflammation and COVID-19. Curr Opin Neurobiol. 2022;76: 102608.
Khairan K, et al. Molecular docking study of fatty acids from Pliek U oil in the inhibition of SARS-CoV-2 protein and enzymes. IOP Conf Ser Mater Sci Eng. 2021. https://doiorg.publicaciones.saludcastillayleon.es/10.1088/1757-899X/1087/1/012058.
Lundstrom K, et al. COVID-19 signalome: pathways for SARS-CoV-2 infection and impact on COVID-19 associated comorbidity. Cell Signal. 2023;101: 110495.
Acknowledgements
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Ministry of Science and ICT (2023R1A2C1007606/ NRF-2022R1A2C2009817).
Funding
There is no funding.
Author information
Authors and Affiliations
Contributions
Sanjeevram Dhandapani: Methodology, Experiments, analyzing RNA sequence, Writing- original draft; Yu Jeong Ha: In vivo mouse experiment, Rongbo Wang: Methodology, Tae Woo Kwon: Data curation, Ik Hyun Cho: Supervision & Editing; Yeon Ju Kim: Project administration, Supervision & Editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The experimental procedures using C57BL/6 mice and Syrian hamsters were approved by the Institutional Animal Care and Use Committee (IACUC) of Kyung Hee University (KHSASP-22-135) and IACUC of Chonbuk National University Hospital (Jeonju-si, Jeollabuk-do, South Korea), respectively.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dhandapani, S., Ha, Y., Wang, R. et al. Lipid-encapsulated gold nanoparticles: an advanced strategy for attenuating the inflammatory response in SARS-CoV-2 infection. J Nanobiotechnol 23, 15 (2025). https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12951-024-03064-5
Received:
Accepted:
Published:
DOI: https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12951-024-03064-5